Biosafety Level 2 Containment Work Practices
Hand Hygiene
- Wash hands upon contact with anything potentially infectious, after work, after removing gloves and before leaving the laboratory
- Gloves are replaced as soon as practical when contaminated, torn, punctured, or when their ability to function as a barrier is compromised
Aerosol Containment
- Perform all procedures in a manner that minimizes splashes, the creation of droplets or aerosols
- Perform procedures that may generate infectious aerosols in a biosafety cabinet
- Use a mechanical pipetting devices at all times
Universal Precautions
- Universal precautions is an approach to infection control in which you treat all human and nonhuman primate blood, tissues and body fluids as if they are potentially infectious for HIV, hepatitis B virus, and other bloodborne pathogens, (Bloodborne Pathogens Standard 29 CFR 1910.1030(b) definitions).
- Implementing universal precautions means that you consistently adhere to
- Hand hygiene
- Wearing non-porous personal protective equipment as a physical barrier between you and the potentially infectious material
- Safe work practices specific to sharps
- Routine surface disinfection
- Waste deactivation and disposal
Delineation of Laboratory from Non-laboratory Operations
- Entry ways to work areas, containers of biohazardous waste, refrigerators and freezers used with potentially infectious materials must have labels with the word “BIOHAZARD” and the universal biohazard symbol in orange-red or red with lettering and symbols in a contrasting color.
- Eating, drinking, smoking, applying cosmetics or lip balm, and handling contact lenses are prohibited in work areas
- Do not handle ear buds or cell phones while wearing PPE
- Food and drink must not be stored in laboratory refrigerators, freezers, shelves, cabinets, or bench tops that contain research material(s)
- Transport biological agents between laboratories and campus buildings using rigid, leak-proof, double container systems that are lined with enough absorbent material to absorb liquid leaks
Disinfection
- Disinfect the work area and lab equipment daily and after use
- Disinfectants don't inactivate microorganisms instantaneously, and the disinfectant needs to dwell on surfaces, e.g., gasketed containers, biosafety cabinet interior, liquid handling equipment used with disposable tips/pipettes, lab surfaces, equipment, safety glasses and face shields
- Use an EPA-registered, high level disinfectant for work with potentially infectious and infectious materials
Housekeeping
- Reduce or eliminate the amount of cardboard
- Take out the recycling and don't allow piles of it to accumulate
- Organize freezer space to ease access and inventory of materials
Written Procedures
- Standard Operating Procedures should be established for techniques, e.g., cell culturing or tissue homogenization, and equipment, e.g., fluorescence activated cell sorters or sonicators
- Methods to prevent occupational exposures are specified by the Principal Investigator within the Biological Use Authorization
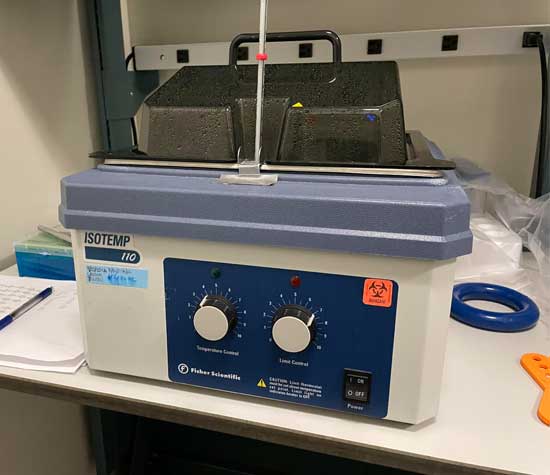
Equipment Decontamination
- You must wear a well-fitted liquid impervious lab coat, along with disposable nitrile gloves, ANSI compliant safety glasses, long pants and closed-toe shoes.
- Most equipment used with biological equipment may be decontaminated by wiping down surfaces with a high-level disinfectant.
- Defrost freezers prior to surface decontamination.
- Biosafety cabinets surfaces are decontaminated before a vapor phase decontamination process by an external vendor. Biosafety cabinets should be decontaminated with a vapor phase process before relocating, moving or re-allocating to new faculty.
- Secondary fungal growth in flasks used for liquid waste deactivation is treated with additional full strength household bleach.
- Removable incubator parts (shelves, racks, humidity pan) may be autoclaved and then wiped down with 70% ethanol.
- Bleach solutions may be dispensed down the sink with an excess of water.
- Remove biohazard labels.
Personal Protective Equipment
- Long pants and closed toe shoes are required for entering and occupying a laboratory
- While working with, or being adjacent to hazardous materials or processes, an appropriate lab coat and safety eyewear are also required
- Wear a cuffed lab coat and disposable gloves when working at a biological safety cabinet
- Wear safety glasses, with an accompanying face shield for handling large volumes for work outside of a biological safety cabinet
- The cuffed, pin-striped barrier lab coats are impervious to small volumes of liquids and are used for work with human blood or other infectious liquid handling procedures
- Lab coats must be visibly clean and laundered as needed
- In case of gross contamination with infectious biological materials, lab coats are to be bagged and autoclaved prior to laundering via Mission Linen
Post Exposure Procedures
- Clean the affected area. Wash needle sticks and cuts with soap and water, flush splashes to the nose, mouth, or skin with water, and irrigate eyes with clean water or sterile saline. The laboratory sink, emergency shower and eye wash stations will be used as necessary to flush affected areas with water for several minutes.
- Report the incident. Exposures must be reported to the PI or Lab Safety Contact immediately. Staff exposures or injuries are recorded with an Employer’s First Report: https://www.ehs.ucsb.edu/workcomp Student exposures or injuries are filed via this webpage: https://www.ehs.ucsb.edu/riskmanagement/incident-reporting
- Seek treatment. Healthcare personnel treating exposed patients must be informed of the biological materials involved in the exposure. Employees and personnel on University pay status seek treatment at Sansum Occupational Medicine Center, 101 South Patterson Avenue, Santa Barbara, CA 93111, and after business hours at Sansum Urgent Care Center, 215 Pesetas Lane, Santa Barbara, CA 93110. Students are to seek treatment at UCSB Student Health Services, Building 588, at El Colegio and Ocean Road, Santa Barbara CA 93117, and after business hours at Goleta Valley Cottage Hospital, 351 S. Patterson Avenue, Goleta CA 93117.
Relocation Guide for Biological Safety
Packing and Transporting Biological Materials across Campus
- Use a rigid, leak-proof, double container system
- Containers must be readily decontaminated, i.e., not Styrofoam or cardboard
- Seal both the inner and outer containers with Parafilm
- Pack items to prevent breakage or leakage
- Line the outer container with enough absorbent material to soak up the volume of liquid
- Do not leave packages unattended
- Label the container with the biohazard symbol and the PI/designee contact information
- Decontaminate the outside of the primary and secondary containers, including any handles, before you exit the lab, so that you can safely doff PPE before exiting
- Bring clean disposable gloves to unpack the container, and carry your lab coat in an unused autoclave bag
Steps to Relocating a Biosafety Cabinet
- Authorized personnel/researchers empty the cabinet and decontaminate interior work areas
- An outside vendor, Technical Safety Services, Inc., performs a decontamination procedure on the entire unit
- UCSB Furniture Services moves the cabinet to the new location, or into surplus
- The PI’s departmental staff finalizes installation
- Technical Safety Services, Inc. recertifies cabinet performance
Sharps Safety
- Limit the use of sharps to circumstances in which there is no alternative
- Uncap needles gently so as to avoid recoil and accidental needlestick
- Keep sharps pointed away from you
- Do not bend, break, shear or remove needles from disposable syringes; dispose of the entire assembly as sharps waste
- Use a one-handed technique if recapping is absolutely necessary; do not recap for disposal
- Plan to dispose of sharps immediately after use; move the sharps waste container so that it's in position beside your bench work, and as near the point-of-use as appropriate
- Do not accumulate used disposable sharps on lab surfaces or in bags
- Dispose of contaminated sharps in a single-use, unlined, disposable container that is rigid, leak proof, puncture resistant, and labeled with the biohazard symbol and “SHARPS WASTE"
- Even safety-engineered sharps must be disposed of within a rigid, lidded and labeled sharps container
- Close the container when it is not in use
- Do not exceed the sharps container fill line at 2/3 full
- Ensure that sharps are contained and do not protrude from the sharps container
- Non-disposable sharps are placed in a hard-walled container for transport to a processing area for decontamination
- Broken glassware is handled with a brush and dustpan, tongs, or forceps
Spill Cleanup
A spill kit, consisting of paper towels, tongs, and disinfectant, is ideally located under or next to the sink. Decontamination of spills within an operating biosafety cabinet proceeds immediately. Keep the cabinet blower on.
- Replace any contaminated personal protective equipment.
- Obtain or prepare a fresh solution of disinfectant.
- Remove any contaminated paper towels and place it into the biohazard bag.
- Cover the area of the spill with new paper towels to prevent aerosols and splashing, and carefully pour disinfectant on the towels, starting from the outside of the spill.
- Allow for the contact time specified for the disinfectant; 20 minutes’ contact time for freshly diluted 10% bleach (final vol/vol).
- Dampen a towel with disinfectant and wipe down the cabinet interior and items inside the BSC.
- Push towels from the edge of the spill to the center and dispose of into a biohazard bag.
- Use paper towels to absorb any remaining liquid, working from the outside in.
- Bag the clean-up materials and disposable gloves as solid waste.
- Change gloves after the work surface is decontaminated and before replacing clean absorbent towels, if used.
- Wash your hands thoroughly.
For larger spills outside of a biosafety cabinet and depending on the materials involved, you may need to vacate the premises for 30 minutes to allow for aerosols to settle and for a few room air exchanges to take place.
- Alert others that there has been a biological spill.
- Remove one glove to open and then close the door behind you, and leave for 30 minutes.
- Remove PPE. Bag contaminated items such as shoes or lab coat for surface decontamination or autoclaving. Wash your hands.
- Post a “Spill Cleanup in Progress” sign at the door warning of the spill and advising of the re-entry time.
Spill Cleanup in Progress
Do not enter the lab.
Re-entry for spill cleanup __:___
This sign will be removed afterwards.
Contact:
- Before entry, put on a fresh lab coat, disposable gloves, and safety glasses.
- Obtain or make a fresh dilution of 10% household bleach (final vol/vol).
- Cover the area with paper towels. Pour (do not spray) 10% bleach on absorbent material in a spiral motion from the outside to the inside. Avoid enlarging the contaminated area.
- Allow for 20 minutes’ contact time.
- While waiting, wipe down nearby stationary equipment and furniture with towels dampened with disinfectant.
- Start at the perimeter and work towards the center to remove towels and place in a biohazard bag.
- Change gloves.
- Clean the area again with towels dampened with disinfectant.
- Remove PPE and wash your hands.
- Inform the lab when cleanup is complete.
- Contact EHS Biosafety to report the spill and inform your PI.
Work with Biological Toxins
- Experiments should be planned to eliminate or minimize work with dry, powdered toxin. Dry toxin must be manipulated using containment equipment such as a disposable glove bag, chemical fume hood or a biological safety cabinet.
- Evaluate and modify experimental procedures to reduce or eliminate the possibility of aerosolizing solutions containing toxin
- For complex operations, new workers may want to perform practice runs in which the procedures are rehearsed without active toxin
- Work with toxins should only be done only in laboratories with controlled access and at pre-determined bench areas. When toxins are in use, the room should be clearly posted: “Toxins in Use—Authorized Personnel Only.”
- Containers used for toxin storage should be sealed, labeled, and secured to ensure restricted access
- Consideration should be given to requiring the presence of at least two knowledgeable individuals at all times in the laboratory for high-risk operations, e.g., manipulations with dry forms of toxins, intentional aerosol formation, and the use of hollow-bore needles in conjunction with amounts of toxin estimated to be lethal for humans
Research groups that uses toxins must augment the laboratory Chemical Hygiene Plan with a Standard Operating Procedure (SOP) for the toxin or class of toxins. The researcher should be sufficiently adept at the planned experimental procedures before working with the toxin.
SOP Components:
- Procurement
- Storage location and security
- Inventory/tracking
- Areas designated for work
- Glove choice based on how the toxin is solubilized (aqueous buffer or organic solvent)
- Methods to transfer liquids containing toxin
- Deactivation methods
- Routine decontamination of laboratory surfaces and equipment
- Solid and liquid waste disposal procedures
- Spill cleanup procedures
UCSB Chemical Hygiene Plan template for work with biological toxins